Written by Hollie Finders, RN
Hollie Finders is a registered nurse with years of experience working in the health care field. She has degrees in both biochemistry and nursing. After working with patients of all ages, Hollie now specializes in pediatric intensive care nursing. Hollie’s LinkedIn
Procedure for Measuring Blood Pressure
Equipment needed: Stethoscope and sphygmomanometer (blood pressure cuff).
- Perform hand hygiene.
- Explain the procedure to the patient and ask for their assistance in following directions.
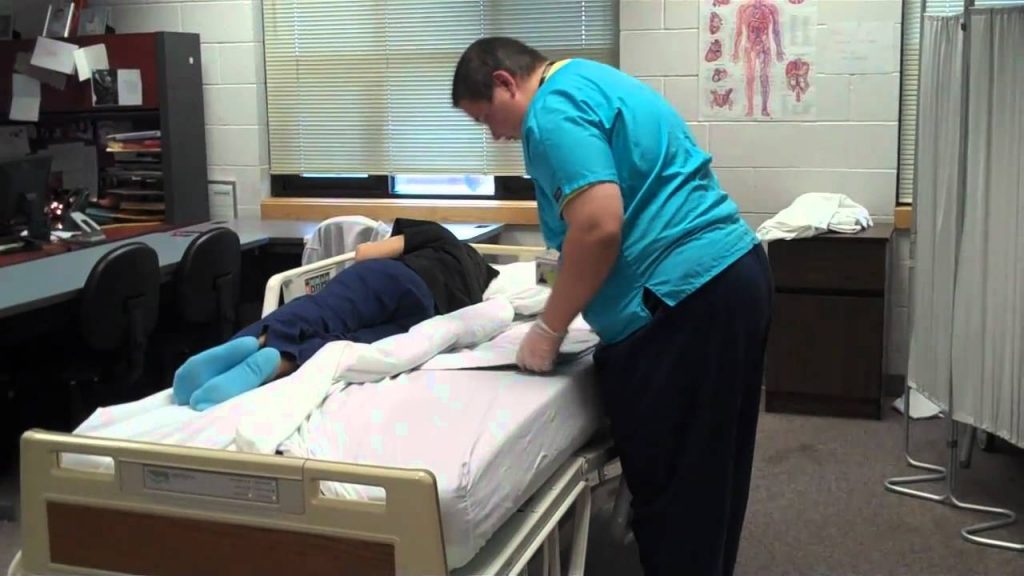
- Assist the patient into a supine or sitting position. Allow the patient to rest in this position for 5 minutes.
- Roll up the patient’s sleeve to expose the patient’s bare arm. Do not attempt to measure blood pressure through clothing.
- Grab the blood pressure cuff, open the valve of the pump, and ensure the cuff is completely deflated.
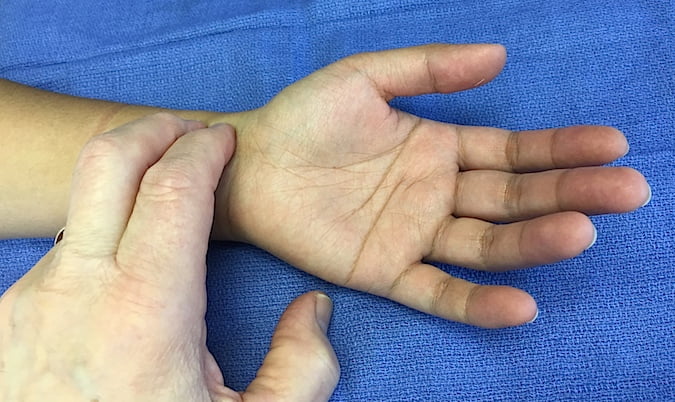
- Locate the pulse of the brachial artery, found in the medial aspect of the antecubital fossa (bend of the elbow). Once found, keep your finger on this spot while you align it with the artery marker on the blood pressure cuff.
- Secure the blood pressure cuff snugly around the patient’s arm, approximately 2 finger widths (1-1.5 inches) above the elbow. Ensure that the cuff is the proper size, taking up 40% of the upper arm.
- Position the arm at the level of the heart with the patient’s palm facing up. If the patient is sitting, make sure the arm is supported.
- Fixate the blood pressure gauge where it can be clearly seen.
- Put the earpieces of the stethoscope in your ears and place the diaphragm of the stethoscope in the antecubital fossa directly over the brachial artery.
- Holding the stethoscope in place with one hand, use your other hand to close the valve of the pump, turning the valve clockwise until it stops. Avoid over-tightening the valve.
- Inflate the cuff quickly to approximately 30 mmHg above the estimated systolic pressure.
- With your thumb and index finger, open the valve just slightly. Allow the cuff to deflate slowly, at a rate of 2 to 3 mmHg per second.
- Watch the gauge closely and note the reading in which the first clear pulse sound is heard. This is the systolic pressure.
- Continue deflating the cuff while watching the gauge. Take note of when the pulse can no longer be heard or when the pulse is no longer distinct and sounds muffled. This is the diastolic pressure.
- Allow the cuff to deflate 10 to 20 mmHg beyond the diastolic pressure and then open the valve completely to deflate the cuff.
- Remove the cuff from the patient’s arm.
- If you miss the systolic or diastolic reading, do not reinflate the cuff. Remove the cuff and wait at least one minute before using the same arm to retake the blood pressure.
- Perform hand hygiene.
- Record the systolic and diastolic pressures, the patient’s position, and which arm was used in the patient’s chart. Notify the nurse of any changes in the patient’s condition.
Important Information about Measuring Blood Pressure
Many factors can interfere with obtaining an accurate blood pressure. The most common mistakes that lead to inaccurate blood pressures are a result of improper technique, including: not supporting the patient’s arm, using the wrong sized cuff, positioning the cuff too low on the patient’s arm, improper positioning of the cuff’s artery marker, and attempting to measure blood pressure through clothing [1]. It is also important to avoid taking a blood pressure in a side that has undergone mastectomy, has paralysis from a stroke, has an IV or dialysis catheter, has had recent trauma, or has severe burns [2,3,4,5].
By: Hollie Finders RN
References
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2911816/
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3652571/
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2399466/